Stereo Implantation of the Thalamus and Cortex in Electrical Status Epilepticus of Sleep: A Pediatric Case Study
Abstract number :
1.355
Submission category :
9. Surgery / 9B. Pediatrics
Year :
2018
Submission ID :
507110
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Ann Hyslop, Nicklaus Children's Hospital; Travis Tierney, Nicklaus Children's Hospital; Ian Miller, Nicklaus Children's Hospital; John Ragheb, Nicklaus Children's Hospital; and Prasanna Jayakar, Nicklaus Children's Hospital
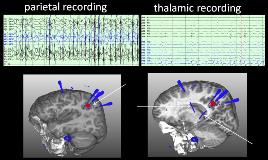
Rationale: Electrical status epilepticus of sleep is a pattern in which there is a significant potentiation of epileptiform activity in the transition from wakefulness to sleep. The incidence is difficult to estimate due to inconsistent inclusion criteria and varying study methodologies. Associated conditions include migrational disorders, shunted hydrocephalus, perinatal vascular lesions, genetic diseases, and thalamic injury. In the context of seizures and neurocognitive regression, this can be referred to as continuous spike wave of sleep (CSWS). Patents with ESES have been found to have a relatively high frequency of thalamic lesions in prior studies. Methods: Case study Results: We report a case of a previously developmentally typical and healthy 4 year old female with left thalamic injury due to a hemorrhage within the first 3 months of life, subtle right hand weakness, 4 lifetime seizures and mild developmental delay that presented with increasing learning difficulties and was found to have ESES on EEG. ESES persisted despite adequate doses of levetiracetam, clobazam, valproic acid, and lacosamide as well as prolonged treatment with high-dose methylprednisolone and high-dose diazepam. Neuropsychological testing performed at age 4, 5, and 6 years of age showed significant declines in multiple domains, including full-scale IQ. Early EEG suggested a region of focal epileptogenicity in the left parieto-occipital region. A presurgical evaluation revealed a focal hypermetabolic region in the left parietal region on PET. She underwent stereo EEG implantation of the left parietal region and anterior and posterior aspects of the injured left thalamic tissue. Extraoperative electrocorticography demonstrated near-continuous epileptiform activity in the left parietal region with a field to the posterior thalamus and propagation to the anterior thalamus (figure 1). Extraoperative thalamic stimulation was performed to determine if the cortical epileptiform discharges could be modulated with stimulation. No significant change was seen in the continuous epileptiform discharges emanating from the cortical electrodes. Therefore, a corticectomy, guided by intraoperative electrocorticography, in the left parietal lobe was performed and ESES resolved post-operatively. Neuropsychological testing performed approximately 1 year later showed improvements in verbal memory, but continued worsening of working memory and full-scale IQ. Subjectively, there was a significant improvement in social and communication skills. At age 8 years, she experienced seizure recurrence and a sleep EEG revealed return of ESES. Conclusions: This case demonstrates the presence of neuropsychological consequences of medically refractory ESES and suggests a possible role of epilepsy surgery in cases with focal EEG, imaging, or functional neuroimaging studies. It also suggests that while thalamic injury can be seen in cases with ESES, the potential role of the thalamus in perpetuation of electrical discharges appreciable in cortical tissue remains unclear. Further study of the neurophysiological mechanisms of ESES is warranted. Funding: None