The Impact of Multimodal 7T MRI in Presurgical Evaluation of Patients With Severe Epilepsy
Abstract number :
3.245
Submission category :
5. Neuro Imaging / 5A. Structural Imaging
Year :
2018
Submission ID :
507105
Source :
www.aesnet.org
Presentation date :
12/3/2018 1:55:12 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Giske Opheim, Copenhagen University Hospital, Rigshospitalet; Melanie Ganz-Benjaminsen, Copenhagen University Hospital, Rigshospitalet; Ulrich Lindberg, Copenhagen University Hospital, Rigshospitalet-Glostrup; Mark B. Vestergaard, Copenhagen University Ho
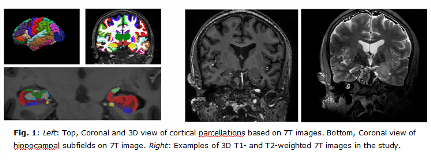
Rationale: One third of epilepsy patients suffer from uncontrolled seizures despite optimal anti-epileptic drug treatment. These patients might be surgical candidates if an epileptogenic focus is identified during the epilepsy surgery evaluation process. Identification of an epileptogenic lesion on MRI at conventional field strengths is considered the most important predictor of a good surgical outcome. The present study will investigate the added clinical value of ultra-high field MRI at 7 Tesla (7T) in the presurgical evaluation of patients included in the Danish Epilepsy Surgery (DES) program. Methods: We recruited 10 epilepsy patients and 14 healthy controls (HCs) that were scanned with the Philips Achieva 7T system. The scan protocol consists of five structural (3D T1 0.7mm iso, 3D T2 0.7mm iso, 3D FLAIR 0.7mm iso, 2D T2 0.5x0.5x0.75mm axial and 0.5x0.5x1mm coronal) scans to match the current 3T MRI protocol. So far, we can present preliminary analysis of cortical thickness- and hippocampal subfield segmentations in Freesurfer 6.0. These computations are based on 3D T1-weighted images, and for hippocampal subfield segmentation, also on an overlay with the 3D T2-weighted images (Fig. 1). Results: Percentage differences in 7T vs 3T hippocampal volumes vary from 0% to 69%, but most volumes for all 10 patients and 14 HCs are within the 40% range. Patient 2, the only patient with mesial temporal sclerosis (MTS), displays significant asymmetry with left whole-hippocampus and all subfields being larger than right side for both 7T and 3T (Fig. 2), consistent with right-sided pathology. Patient 5, a patient with right-sided neocortical polymicrogyria as the only clinical finding on 3T MRI, displays hippocampal asymmetry with all right-sided subfields and whole hippocampus being larger than the left-sided on the 7T image, while only three right-sided subfields are significantly larger on the 3T image. Results from cortical parcellations display variabilities in thickness, asymmetries between hemispheres, and 7T vs 3T differences for all patients and HCs, similar to those from patient 2 on Fig. 2. Conclusions: These preliminary analyses demonstrate the potential for further assessment of automatically segmented cortical thickness and hippocampal subfields in epilepsy patients. The current sample size is too small to do a quantitative analysis and use results for, e.g., model training or explanation of 7T vs 3T differences in thickness and volumes. We will continue the inclusion of epilepsy patients additional to these patients included in April and May 2018, and expect to present data on other features, such as regional cortical volumetry measures and local- and whole-brain connectivity in surgery candidates with a variety of epileptogenic lesions. Funding: Danish Council for Independent Research: DFF–7016-00151The Lundbeck Foundation: R280-2017-3925
.tmb-.png?Culture=en&sfvrsn=816daa57_0)