Treatment of KCNB1-Related Epilepsy: A Parent Survey
Abstract number :
1.309
Submission category :
7. Antiepileptic Drugs / 7C. Cohort Studies
Year :
2018
Submission ID :
502025
Source :
www.aesnet.org
Presentation date :
12/1/2018 6:00:00 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
John B. O'Connor, Lurie Children's Hospital of Chicago; Sam Kang, Northwestern University Feinberg School of Medicine; Emily M. Bryant, Lurie Children's Hospital of Chicago; Anne T. Berg, Ann & Robert H. Lurie Children's Hospital of Chicago; Jennifer A. K
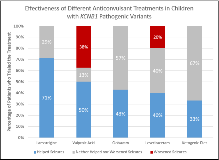
Rationale: Pathogenic variants identified in the KCNB1 gene, which codes for the voltage gated potassium channel, Kv2.1, have been associated with a severe form of early life encephalopathic epilepsy. KCNB1-related epilepsy is extremely rare, likely < 200 cases per year in the US. Consequently, there is currently no rigorous evidence upon which to base seizure treatment. With such rare conditions, initial understanding of likely best drug choice often comes from review of case series. Methods: Children with pathogenic KCNB1 variants were recruited into a study of epileptic channelopathies. Parents reported information regarding seizure onset, genetic variants, medications used for seizures and response to those medications. Parents also provided a copy of their child’s genetic testing report. Results: In 16 children (10 female, 6 male), many parents reported multiple seizure types with the median number of 4.5 different types (IQR=2.5 to 6). 75% (N=12) reported their child having absence seizures, 63% (N=10) reported generalized convulsions, 56% (N=9) reported focal or hemi-convulsions, 56% (N=9) reported myoclonic seizures, 56% (N=9) reported tonic seizures, 50% (N=8) reported atonic or drop seizures, and 13% (N=2) reported infantile spasms. In the cohort of children, the 5 most commonly trialed medications were levetiracetam (N=11), clobazam (N=8), lamotrigine (N=8), valproic acid (N=8), and the ketogenic diet (N=4). If parents reported both improved and worsened seizures (N=5) the drug trial was omitted due to ambiguity. The highest number of beneficial responses was for lamotrigine (71%), and the lowest was for the ketogenic diet (33%) (p=0.95) (Figure 1). Valproic acid had the highest incidence of negative response, with 38% of parents reporting it made seizures worse (Figure 1). Conclusions: Most children with KCNB1-related epilepsy experience a diverse array of seizure types, with the majority of subjects experiencing generalized convulsions and absence seizures. Due to the wide range of seizure semiology experienced, it is expected that many different medications would be tried with differing degrees of efficacy. Lamotrigine appeared to be the most beneficial anticonvulsant in this cohort and valproic acid appeared to be the most harmful to the point of exacerbating seizures. Further investigation into these findings is needed in prospective comparative effectiveness studies coupled with an understanding of drug mechanisms and functional impact of the different KCNB1 variants. Funding: No funding was received in support of this abstract.