Treatment of Medically Refractory Seizures Associated With Tuberous Sclerosis by RNS System
Abstract number :
2.139
Submission category :
4. Clinical Epilepsy / 4C. Clinical Treatments
Year :
2018
Submission ID :
501587
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Ning Zhong, Kaiser Permanente Sacramento Medical Center and Dorris D. Luong, Kaiser Permanente Sacramento Center
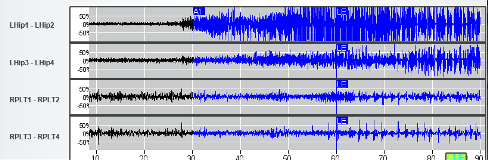
Rationale: The prevalence of epilepsy in Tuberous Sclerosis Complex (TSC) is 80-90%, of which substantial proportion being pharmacoresistant focal or multifocal seizures. Epilepsy surgery (resecting epileptogenic tuber(s) or laser ablation) is performed in less than 10% of such patients. Other palliative surgical options, such as VNS implantation, or corpus callosotomy, have been utilized when resection not possible. The responsive neurostimulation system (RNS), is a safe and effective option for focal onset (= 2 foci) seizures. Clinical data of utilizing RNS for seizure treatment in TSC patient is limited. We reported the evaluation and treatment with RNS in a TSC patient. Methods: Presurgical workup with video EEG (vEEG) monitoring, brain MRI and PET scan, neuropsychology exam, and intracranial EEG monitoring were reviewed. Post-RNS-implantation EcoG data and treatment outcome were analyzed. Results: 22-year-old man with TSC had first seizure at 12-years age, presented as blank starring, generalized tonic-clonic seizure. When the patient was referred to our comprehensive epilepsy center at age 20 year, he was on four antiepileptics. He still had three different seizure types, 1) aura, feeling weird in his throat or head, with frequency 1-2 time weekly; 2) seizures with impaired awareness, starring straight, incoherent speech or not able to answer questions, amnestic to episodes; happening once a month; 3) rare generalized convulsion. vEEG monitoring recorded multiple focal onset seizures independently arising from bilateral temporal regions. Brain PET showed hypometabolism in bilateral temporal regions, which being compatible to vEEG results. Brain MRI showed scattered tubers, subependymoma nodule, and subependymal giant cell astrocytoma. However none of such pathology co-localizing with the seizure onsets. Invasive monitoring confirmed focal seizures arising independently from the left hippocampus and the right posterolateral temporal lobe with rapid spread to the right hippocampus. Given bilateral onsets, it was decided to proceed with RNS implantation, bilateral hippocampal depth electrodes and a lateral right temporal subdural strip were placed. RNS stimulation was turned on after a month data collection, bilateral seizure patterns were confirmed (Fig 1 & 2). At the 6 months follow-up, he reported 12 clinical events (4 seizures and 8 auras) during the interval, seizure frequency dramatically decreased and less seizure severity was also reported. RNS recorded 44 electrographic seizures, 77% of which arising from the left hippocampus. RNS delivered the therapy, and 45% of the detected seizures were successfully terminated. Conclusions: The patient tolerated well with the RNS implantation procedure and the stimulation treatment. The efficacy of RNS treating seizures within 6 months post-implantation interval was compatible with the reported clinical trial data. Our data added important observation of utilizing RNS for seizure control in selected TSC associated epilepsy patients. Through comprehensive pre-surgical workup, seizure onset focus (foci) can be identified. RNS can achieve good seizure control in such highly selected patients when surgical resection not possible. Funding: None
.tmb-.png?Culture=en&sfvrsn=da0a6b9a_0)