VNS Associated Sleep-Disordered Breathing in Pediatrics: Prospective Analysis
Abstract number :
2.320
Submission category :
9. Surgery / 9B. Pediatrics
Year :
2018
Submission ID :
495106
Source :
www.aesnet.org
Presentation date :
12/2/2018 4:04:48 PM
Published date :
Nov 5, 2018, 18:00 PM
Authors :
Christopher Carosella, Cincinnati Children’s Hospital Medical Center; Narong Simakajornboon, Cincinnati Children’s Hospital Medical Center; David Smith, Cincinnati Children’s Hospital Medical Center; and Thomas Dye, Cincinnati Children&#
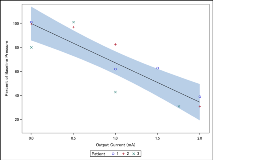
Rationale: Vagal Nerve Stimulators (VNS) are implantable devices used for seizure palliation in intractable epilepsy. Case studies have documented sleep-disordered breathing (SDB) in association with VNS treatment in both adult and pediatric patients. These reports have also shown that standard of care treatments may not be effective in patients suffering from VNS associated SDB, and a high percentage may be resistant to treatment with positive airway pressure. There is emerging evidence that adjustment of VNS settings may provide improvement in VNS associated SDB. However, the type, timing, and consequences of adjustments have not been studied in a systematic, prospective manner. Methods: Patients with documented VNS associated SDB meeting study inclusion and exclusion criteria underwent polysomnography (PSG). During PSG evaluation, standardized adjustments were made to VNS settings including output current, duty cycle (off time duration), pulse width, and frequency. Maximal VNS settings for each subject were defined as the most recent stable home VNS settings. During PSG, VNS adjustments were monitored for 15 minute epochs. These epochs were analyzed for presence and severity of SDB. Apneas and hypopneas were scored according to the AASM Manual for the Scoring of Sleep and Associated Events . Analysis of the nasal pressure waveform was used to assess airflow during VNS on time and VNS off time. Changes in airflow were calculated by comparing the mean of the peak pressure signals during on time to the mean of the peak pressure signals during off time. Reduction in airflow was used as a surrogate for respiratory obstruction. Results: PSG data was obtained from three subjects, two male and one female. Ages ranged from 11-16 years with an average of 12.7 years of age. PSG demonstrated a significant linear inverse correlation between mean airflow and VNS output current, with an average decrease of 18.1% in nasal airflow during on time as compared to off time for each 0.5 mA increase in output current (r2=0.817, p=0.0003). AHI and OI did not differ significantly across adjustment epochs, p = 0.97 and p = 0.69, respectively. Conclusions: This pilot study is the first to prospectively evaluate the association between discharge during VNS on time and SDB in a pediatric population. Preliminary results demonstrate a linear association between VNS parameters and the degree of respiratory obstruction, as measured by nasal pressure transducer. Specifically, we found that as output current increased, airflow decreased. Other measures such as esophageal pressure monitoring may be helpful in the future to evaluate VNS associated respiratory events during sleep. Funding: This study was supported by the Cincinnati Children’s Research Foundation.